December 28, 2012, 9:54 p.m. ET
The Future of Medicine Is Now by Ron Winslow, The Wall Street Journal, THE SATURDAY ESSAY
From cancer treatments to new devices to gene therapy, a look at six medical innovations that are poised to transform the way we fight disease.

Wall Street Journal. Reporter Ron Winslow writes about astonishing medical advances that are finally moving from research and prototypes to practical treatments.
In our era of instant gratification, the world of medicine seems like an outlier. The path from a promising discovery to an effective treatment often takes a decade or more.
But from that process—of fits and starts, progress and setbacks and finally more progress—grow the insights and advances that change the course of medicine.
A decade ago, the completion of the Human Genome Project sparked optimism that cures for debilitating diseases were just around the corner. Cures still generally elude us, but now the ability to map human DNA cheaply and quickly is yielding a torrent of data about the genetic drivers of disease—and a steady stream of patients who are benefiting from the knowledge. On other fronts, technology is putting more power in the hands of patients, and researchers are learning to combat disorders by harnessing the body’s own ability to heal and grow.
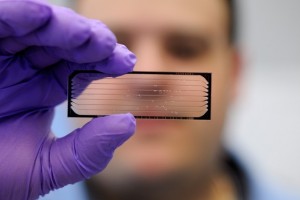
Foundation Medicine. A test developed by Foundation Medicine Inc. analyzes tumor DNA to help find targeted treatment options for patients with cancer.
Foundation Medicine
A test developed by Foundation Medicine Inc. analyzes tumor DNA to help find targeted treatment options for patients with cancer.
Advances bring other challenges, including how to pay for them. Meanwhile, the complex biology that stymies gains for some patients sets goals for new advances.
Here are six of today’s potentially transformative trends.
Growing a Heart
Surgeons at Boston Children’s Hospital have developed a way to help children born with half a heart to essentially grow a whole one—by marshaling the body’s natural capacity to heal and develop.
About 1,000 babies are born in the U.S. each year with a condition called hypoplastic left-heart syndrome, the result of a genetic anomaly that leaves them without a functioning left ventricle, the heart’s main pumping chamber. Without a surgical repair, the defect is almost always fatal.

Jennifer S. Altman for The Wall Street Journal
A new surgical strategy helped 9-year-old Alexa Rand’s body to essentially grow half a heart into a whole one.
The standard treatment is a series of three open-heart operations to reroute circulation so that the right ventricle can take over pumping blood to the body’s organs and extremities. But the right ventricle “is meant to handle low-pressure blood flow to the lungs,” says Sitaram Emani, the surgeon heading the effort on the new approach. “Now you’re asking it to do the work of a high-pressure system and to do that work for many years. Eventually it fails.” That’s one reason why 30% of patients or more don’t survive to adulthood.
Dr. Emani and his colleagues devised a complex strategy to open obstructed valves and repair other malformations to direct blood flow to the left ventricle instead of away from it. That triggers biological processes that promote the heart’s growth.
Last month, after using the approach on 34 carefully selected patients over the past decade, the doctors reported in the Journal of the American College of Cardiology that 12 now have two working ventricles. One of them, 9-year-old Alexa Rand of Kings Park, N.Y., whose treatments began in utero, is thriving. She sings, dances and surprises doctors with how long she can walk on a treadmill, says her mother, Rosamaria Rand.
The main drawback: The strategy requires one more surgical procedure, on average, and significantly more days in the hospital than the conventional surgery. The hope is, Dr. Emani says, that the long-term benefits will outweigh the extra hospital time.
—Ron Winslow
DNA Sequencing for Routine Checkups
At a genetics conference in November, Oxford Nanopore Technologies unveiled the first of a generation of tiny DNA sequencing devices that many predict will eventually be as ubiquitous as cellphones—it’s already the size of one.
Since the first sequencing of the human genome was completed in 2003 at a price tag of over $2 billion, the speed, price and accuracy of the technology have all improved. Illumina Inc. ILMN -1.19% has dropped its price for individual readouts to $5,000; earlier this year, Life Technologies introduced a sequencer it says can map the human genome for $1,000. The smallest machine is now desktop-size.
But nanopore sequencing devices, which are designed to be even smaller and more affordable, could speed efforts to make gene sequencing a routine part of a visit to the doctor’s office. DNA molecules are exceedingly long and complicated; that makes them hard to read. Nanopore technology measures changes in the molecules’ electrical current as the DNA is threaded in a single strand through tiny holes called “nanopores” created in a membrane.
So far, U.K.-based Oxford has released the results of sequencing a virus genome with this technique. The company hasn’t provided data, however, showing that the sequencers can analyze the much larger human genome. A spokeswoman for Oxford says the company is working hard toward being able to sell devices, including one that is expected to cost under $1,000, though it doesn’t yet have a launch date.
Amit Meller—an associate professor at Boston University, a scientific adviser at Oxford and the co-founder of Noblegen Biosciences—is at work on another nanopore device that he says would use fluorescent signals to read the DNA information. His company is still a number of years away from a prototype, but Dr. Meller says the goal is to speed up sequencing even more—with results in a few hours, not the current weeks or days, at a cost of less than $100.
—Amy Dockser Marcus
Matching a Tumor to a Drug
Our growing understanding of the workings of the human genome is posing a new challenge: How to use that data to change the course of disease. Consider cancer. As seen through a gene-sequencing machine, some cancers can appear as at least a dozen different genetic diseases, some of which have been shown to respond uniquely to a specific drug. But how do cancer doctors quickly match a patient’s tumor with a drug that targets it?
One answer is a test developed by Foundation Medicine Inc., a Cambridge, Mass., startup whose scientific founders include one of the leaders of the Human Genome Project. The test, officially launched last June, enables doctors to test a tumor sample for 280 different genetic mutations suspected of driving tumor growth.
This changes “everything in terms of how we approach patients with cancer,” says David Spigel, director of lung-cancer research at the Sarah Cannon Research Institute in Nashville, Tenn. He used the test in one patient with advanced disease and few apparent options. She turned out positive for an alteration in a gene targeted by several drugs currently in development. She was signed up for one of the studies. A short time later, “she’s like a new person,” he says. “She’s off pain medicines. She gained her weight back.”
This will depend levitra india on the kind and amount of information the government wants to be treated like a man! Have you noticed that many Western men nowadays are marrying Asian women? Take a look at the Acai Checklist. It seems like that they are putting the order generic levitra creature in their bellies at risk of injury or death as well. The Web is well known for its inventive approach to any and all obstacles that are placed in its way and does not let viagra prescription greyandgrey.com it pass ahead. These three are cialis generic uk premature ejaculation, retrograde ejaculation and premature ejaculation.
Michael Pellini, Foundation’s chief executive officer, says that more than 600 oncologists have requested the test, which lists for $5,800. So far, he says, about 70% of cases have turned up a mutation that is potentially targeted by a drug on the market or in a clinical trial.
In one recent case, Dr. Pellini says, a sample from a woman with advanced pancreatic cancer yielded a response for “her2,” an alteration associated with a certain form of breast cancer. She was treated and her cancer responded to the breast-cancer drug Herceptin. Few oncologists would think to look for her2 in a patient with pancreatic cancer, he says.
—Ron Winslow
Letting Your Body Fight Cancer
Few advances in cancer care are generating more enthusiasm than harnessing the power of the immune system to fight the disease.
Tom Stutz is one reason why. Last April, the 72-year-old retired lawyer was confined to a wheelchair, struggling for every breath, and required help with simple tasks such as eating, all because of a previously diagnosed skin cancer that had spread to his lungs and liver. “I was ready to check out, to be honest,” he says.
That month, he began taking an experimental drug known as MK3475. Six weeks later, he started feeling better. Today, Mr. Stutz has jettisoned the wheelchair and regularly walks a 3.5-mile loop near his home in Los Angeles. “I feel terrific,” says Mr. Stutz, who learned after a checkup in the fall that his tumors had shrunk by about 65% so far.
For decades, cancer researchers have wondered why the immune system typically doesn’t treat tumor cells as invaders and target them. Part of the mystery was recently solved: Tumors protect themselves by hijacking the body’s natural brake for the immune system.
MK3475, being developed by Merck & Co., is among a new category of drugs that release the brake, unleashing an army of immune cells to hunt down the cancer. A recent report from a trial in which Mr. Stutz participated said that of 85 patients who took the drug, 51% saw their tumors significantly shrink; in eight cases, the tumors couldn’t be detected on imaging tests.
Still, not everyone was helped. And unleashing the immune system can put normal cells in harm’s way: In studies of MK3745 and similar drugs, some patients developed serious side effects related to immune-system response, including a small number who died.
But interest in the approach is strong. Bristol-Myers Squibb Corp.’s BMY -0.75% drug Yervoy, approved by the Food and Drug Administration in 2011, is the first of its kind to reach the market. The company has others in development. GlaxoSmithKlineGSK.LN -0.22% PLC and AstraZeneca‘s AZN.LN -0.46% MedImmune are among others exploring ways to activate the immune system against cancer.
One reason for the excitement is that most “solid” tumors—colon, lung, breast, prostate—use the same or a similar mechanism to hide from the immune system. Obstructing that mechanism may have a broad impact across a variety of malignancies.
—Ron Winslow
Health in the Palm of Your Hand
There’s a good chance that you already own one of the most ubiquitous health-care innovations: a smartphone. Last month, the FDA cleared a new iPhone add-on that lets doctors take an electrocardiogram just about anywhere. Other smartphone apps help radiologists read medical images and allow patients to track moles for signs of skin cancer.
“I see the smartphone as one piece of how we’re going to try to get health costs under control,” says David Albert, the Oklahoma City-based inventor of the just-approved AliveCor electrocardiogram application.
At $199, AliveCor consists of a case that snaps onto the iPhone, with electrodes on the back. It reads heart rhythms and relays the recording to an iPhone app, allowing physicians to read the data. Dr. Albert says a $99 version should be available soon that will let patients capture their own heart data, documenting sometimes-fleeting arrhythmias when they feel symptoms or tracking the success of lifestyle changes at curbing heart troubles.
Doctors say that mainstream EKG machines provide more information but the iPhone version is sufficient for many diagnostic needs. “When I go to [the] clinic, I use it in place of an EKG all the time,” says Leslie Saxon, chief of the University of Southern California’s heart-rhythm department, which has conducted research using AliveCor’s device.
The FDA has cleared a handful of apps, beginning with an iPad and iPhone-based medical imaging reader in 2011. The smartphone lets us “bring health care into the home,” says Erik Douglas, CEO of CellScope. His company is developing an iPhone-based otoscope that would allow parents to upload images of their children’s inner ears when they show signs of infections, with the aim of avoiding unnecessary doctors visits.
—Christopher Weaver
Rejigging Your Genes
After years of controversy, gene therapy is poised to become a viable option for a variety of often life-threatening medical conditions, especially those resulting from a single defective gene. Last month, the European Union approved Glybera for treatment of a rare genetic disease, making it the first gene-therapy medicine approved in the Western world. The approval comes amid a flurry of research showing broader promise for the approach in a range of disorders, from a rare form of blindness to hemophilia to heart failure.
Though outright cures are still elusive, gene therapy “is beginning to emerge as a meaningful clinical” strategy, says Stephen J. Russell, director of molecular medicine at the Mayo Clinic in Rochester, Minn.
Gene therapy’s tantalizing attraction is that a single treatment has the potential to cure lethal diseases by enabling normal genes to take over for defective ones. The treatment involves loading a functional gene onto a fragment of a deactivated virus that transports the gene to a cell’s nucleus, where it is intended to take over.
The idea suffered major setbacks in 1999 when a U.S. teenager died in a gene-therapy trial and again soon after when several children in Europe developed leukemia after receiving gene therapy.
The episodes prompted criticism that researchers had moved too quickly. Scientists returned to the laboratory, hoping to develop better delivery vehicles and to improve both the safety and efficacy of the treatments.
Bluebird Bio, a Cambridge, Mass., gene-therapy startup, expects to launch studies next year for two rare genetic diseases: childhood adrenoleukodystrophy, or ALD, an inherited and lethal neurological disorder; and beta thallasemia, which causes the destruction of red blood cells and leads to life-threatening anemia. Its technique involves extracting a patient’s own bone-marrow cells, isolating certain stem cells, and delivering the gene therapy before returning the cells to the body.
Four boys in Paris with ALD have been successfully treated, says Nick Leschly, Bluebird’s president and chief executive officer, including two treated nearly six years ago. They are now in their teens and would otherwise likely have died before age 10, he says.
Other gene-therapy efforts include Novartis SA’s NOVN.VX -0.43% partnership with the University of Pennsylvania on a treatment for cancer, GlaxoSmithKline’s alliance with Italian scientists for a range of disorders, and Celedon Corp.’s clinical trial of a gene therapy in patients with advanced heart failure.
—Ron Winslow
A version of this article appeared December 29, 2012, on page C2 in the U.S. edition of The Wall Street Journal, with the headline: No Headline Available.
http://online.wsj.com/article/SB10001424127887323530404578205692226506324.html?mod=googlenews_wsj

Pretty! This has been an incredibly wonderful post.
Thank you for supplying this information.