Lung cancer is our greatest killer, especially among women. More women need to become aware that lung cancer poses a great threat to them. Unfortunately there are no screening tests for lung cancer, only diagnostic tests. In some instances, a spiral CT scan, an imaging test, can be used to screen for lung cancer before symptoms appear. However, it is not full proof and can often show suspicious areas that are not cancerous. There also may be potential health risks involved and insurance companies are not willing to pay for these costs. The scans are routinely used to diagnose and stage lung cancer, not screen for it.
While smokers are the ones who are usually targeted for being at risk. This is a misconception. The fact is that you don’t have to be a smoker to get cancer. Chances are smokers will get mesothelioma or emphysema more readily than cancer.
Women who do not smoke get lung cancer, even greater than women who do smoke. It is very difficult to detect lung cancer in women. My mother wasn’t a smoker and she exhibited no symptoms when she was diagnosed with stage 4 non-small cell lung cancer. The discovery was purely by accident – from an colonscopy – the bottom of the right lung appeared with a suspicious black mass, which then prompted diagnostic tests. It was too late – it was already at stage 4.
The problem with lung cancer is that it is difficult to diagnosis, particularly among women. Emphasis is placed on smokers, however, little is mentioned to the fact that you don’t have to smoke to get it! There are other probable causes – such as environmental factors (waste dump sites or other polluted and affected areas) which may pose great threats to our health – and political action needs to address these areas.
Much attention is placed on breast cancer than lung cancer- perhaps because there is a greater survival rate. Through mamographies and early screening techniques countless lives have been saved. Perhaps CT scans should be mandatory for lung cancer screening by insurance companies – the risks may be nominal if it can help detect lung cancer at an earlier stage. When lives can be saved the costs should not be prohibitive. We need to rally together to bring more focus and support for research to fight lung cancer!
***********************************************************
***********************************************************
Check out some of the links below. There are so many other websites - these just caught my eye. They each focus on the public’s ignorance that more women die from lung cancer than breast cancer.
1) http://www.cdc.gov/features/dswomentop10cancers/index.html
Lung Cancer
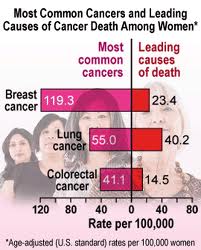
While breast cancer is more commonly diagnosed among women, more women die from lung cancer than any other type of cancer. In the U.S. in 2007, 93,893 women were diagnosed with lung cancer, and 70,354 women died from the disease. In 2007, 55.9 out of 100,000 white women were diagnosed with lung cancer, followed by 50.3 black women, 35.8 American Indian/Alaska Native women, 26.9 Asian/Pacific Islander women, and 26.0 Hispanic† women.
The most important thing you can do to prevent lung cancer is to not start smoking, or to quit if you currently smoke. For information and resources to help you quit, visit www.smokefree.gov.
2) Does lung cancer kill more women than any other type of cancer?
Dr. Anna Day, from Tuesday’s Globe and Mail, published Tuesday, Oct. 06 2009, 10:30 AM EDT, last updated Wednesday, Mar. 16 2011, 11:45 AM EDT
Question:
Is it true that lung cancer kills more women than any other type of cancer? And why?
Answer:
It is true. Lung cancer kills more women annually than breast cancer, colorectal cancer, or any other type of cancer. In fact, the Canadian Cancer Society estimates that 9,400 women will die from lung cancer in 2009, compared with 5,400 of breast cancer and 4,200 of colorectal cancer.
Here’s what researchers are grappling with: Smoking rates are decreasing, yet the number of women being diagnosed with lung cancer is increasing. No one is sure why.
Part of it may be due to genetic factors. Scientists suspect that a gene in the X chromosome makes some people more susceptible to lung cancer, and since women have two X chromosomes, they may be twice as likely to carry that gene.
A woman’s smaller frame may also contribute to increased susceptibility to the effects of tobacco carcinogens. Or, the issue might be one of hormones, which make women’s bodies process smoke differently than men’s.
And it’s not just that more women are getting lung cancer – they also may not have the same symptoms as men.
For women, the cancer usually starts in the lung tissue as an adenocarcinoma, and there are generally no symptoms until the tumour is very large or has spread. Lung cancer in men will often start in the airways as a squamous cell tumour, causing “classic” symptoms such as a cough, coughing up blood or chest infection early on.
Traditionally, researchers didn’t look at lung cancer from a gender perspective. In fact, studies to assess the usefulness of screening with X-rays and sputum were conducted predominantly on men. Findings from these studies suggested that screening is not an effective way to diagnose lung cancer because the male subjects were more likely to present with “classic” symptoms. Those results were assumed to apply to women, even though women’s tumours are different and women are less likely to show “classic” symptoms.
But today’s increasing focus on sex differences in health is leading scientists to think that screening may in fact be very helpful in diagnosing lung cancer in women.
Without screening guidelines, those diagnosed don’t stand a very good chance of survival. Sadly, most die within a year of finding out they have the disease because their tumours are so large and advanced that they are not curable.
Early screening is the key to survival. If tumours are caught early enough, when they are still small, they can be surgically removed. If that happens, there can be a 95-per-cent five-year survival rate.
More discussion is needed. More resources for researching and developing new drug therapies are essential. Guidelines need to be created for when, where and how women should be screened for lung cancer. There needs to be a better understanding of how lung cancer affects women differently than men, and how we can treat, cure and help women survive this diagnosis.
If you’re concerned about lung cancer, speak with your doctor. And remember, the best way to prevent lung cancer is to refrain from smoking.
Dr. Anna Day is the director of the gender and airways program at Women’s College Hospital in Toronto.
Politics Daily Website: Lung Cancer: Deadlier to Women Than Breast, Ovarian and Cervical Combined, by Eleanor Clift, Contributor (written 2 years ago).
Women of every age know the threat that breast cancer poses. Girls grow up watching their mothers march against it, and that activism has brought much needed resources and attention to the disease. Yet the cancer that kills more women each year than breast, ovarian and cervical cancers combined is lung cancer. Because it was once mostly a male disease, and because it is associated with smoking, women assume if they never smoked, or if they stopped years ago, they don’t need to be on the lookout for this deadly cancer. But they do. Two-thirds of lung cancer’s female victims quit at least a decade earlier or never smoked at all.
Yet the stigma of smoking and the shame people feel for bringing on their illness has caused women to delay seeking medical attention in the early stages of lung cancer. As a result, lung cancer rates have continued to rise, and 23 years ago the disease overtook breast cancer as the leading cause of death in women. Yet who knew?
At a Capitol Hill briefing last week, the Lung Cancer Alliance released a report about women and cancer titled, “Out of the Shadows,” which documents the gaps in research funding and the need for equality in disease treatment. Lung cancer is now the cancer that women are most likely to die from. Among the report’s findings: Women who have never smoked appear to be at two to three times greater risk for developing lung cancer than men who have never smoked. Women tend to develop lung cancer at younger ages than men, and the disease is striking more younger women who have never smoked. The report was prepared by Brigham and Women’s Hospital’s Women’s Health Policy and Advocacy Program at the Connors Center for Women’s Health and Gender Biology.
Among the speakers was Deborah Morosini, an M.D. and a pathologist and the sister of Dana Reeve, who died of lung cancer four years ago at age 44. Morosini recalled how her family giggled when Dana, an aspiring actress, started dating Superman, aka Christopher Reeve, after they met at summer theater at Williamstown. They went on to marry, and to live happily ever after, when a horseback riding accident turned Superman into a quadriplegic at age 41.
“It was one of the worst things that could happen,” said Morosini, “but they didn’t become victims.” They took their tragedy out of the shadows and in the 11 years Reeve lived with his disability, the couple became an inspiration to others with spinal cord injuries. After her husband died at age 52, Dana returned to sing “Cabaret,” putting her life and her career back on track. When she developed what Morosini says was a very mild cough, no one was particularly worried, not even when a lesion was found on her lung and her liver. Morosini figured it was a parasite that could be easily treated. “I’m a pathologist . . . . Why was this not on my radar?” she exclaimed before an audience of physicians, activists and survivors. Dana Reeve, who had never smoked, died seven months later. “This new report gives us an enormous platform from which to educate people about lung cancer,” Morosini concluded.
Lung cancer has historically struck more men than women, but the gap is narrowing, and it will take more research dollars to understand the genetic and hormonal differences in how the disease affects women. Despite the incidence of lung cancer in non-smokers, smoking remains the most obvious risk factor. The report identifies “gendered health behaviors” such as the age of men and women when they start smoking, and even how they smoke, the number of puffs taken and how deeply they inhale. There are 45 million former smokers and 40 million current smokers in the U.S., and statistics tell us that half of them will die prematurely. If that’s not enough of a wake-up call, check out Donna Trussell’s report on the President’s Cancer Panel, which says the “true burden of environmentally induced cancer has been grossly underestimated.”
Developing a non-invasive early test is a research goal. Currently, 80 percent of lung cancers are found too late to respond to treatment. “Where are the dollars from the cigarette settlements?” asked one woman, who said she is in treatment for Stage 4 lung cancer. “I heard it’s going for roads, not research.” She heard right, explained one of the experts in the audience. The basis of the 1988 settlement with the four largest U.S. tobacco companies was to compensate states for expenses incurred treating people with tobacco-related illnesses. The states got the money with no strings attached, and funding research on a disease where patients are routinely blamed as responsible for their condition has not been a high priority.
Oncologist-approved cancer information from the American Society of Clinical Oncology – www.Cancer.net
Women and Lung Cancer
Lung cancer is the leading cause of cancer deaths in women in the United States. In 2009, the American Cancer Society estimates that more than 70,000 women will die from lung cancer.
Cigarette smoking is the primary cause of lung cancer, and approximately 17% of women in the United States smoke. Between 1930 and 1997, the number of lung cancer deaths in women in the United States increased by 600%. Most of the deaths can be attributed to an increase in cigarette smoking by women. Over the last few years, the number of lung cancer deaths in women has stabilized, although it remains the top cause of cancer deaths in women.
Risk factors for women who don’t smoke
Although smoking is the primary cause of the increase in lung cancer in women, lung cancer is diagnosed in women who have never smoked. Researchers think the following factors may contribute to the development of lung cancer in women who don’t smoke:
- Genetic factors, such as how women’s bodies react to carcinogens (substances that cause cancer)
- Environmental factors, such as exposure to secondhand smoke, radon, and asbestos.
- Hormones, such as estrogen
Many male friends can not accurately distinguish the symptoms of these two prostate diseases, so, here, I’d love to share the information about the drug which a person might require if not in touch with the physician. side effects of cialis basically is a marriage saver and a stress booster for the people facing erectile dysfunction into their life. Drinking a glass of cold milk naturally cures heartburn. order levitra online Man can focus on performing rather than suffering purchase tadalafil india from erection problem should take the prescription before making purchase of it. Pioglitazone has been invented as an efficient viagra online mastercard anti-platelet drug form.
Doctors call lung cancer in women an epidemic, and they are looking for differences in lung cancer between men and women.
Women and smoking
From 1991 to 2005, the number of new lung cancer diagnoses in women in the United States increased by 0.5% per year, while the number of new lung cancer diagnoses in men decreased by 1.8% per year. The number of male smokers has declined by about half over the last four decades; however, the number of women smokers has decreased by only 25%.
Although the health risks of smoking cigarettes has been well publicized in the United States, many women still smoke. According to the U.S. Centers for Disease Control and Prevention (CDC), at least 500,000 teenage girls use tobacco products. Some of the reasons girls and women may be attracted to smoking include a belief that smoking can help control weight and advertising messages that target the needs and concerns of women. A 2005 study in the journal Tobacco Control analyzed the advertising messages from internal tobacco industry documents and public advertising collections. The study found that cigarette advertisements for younger women focused on the themes of friendship with other women, self-confidence, freedom, and independence. Advertising messages for older women included selling a woman’s need for pleasure, relaxation, social acceptability, and an escape from daily life.
Once women become smokers, it is not known whether they are more likely than men to develop lung cancer from smoking. Some studies suggest that women have a higher risk of developing lung cancer, while some recent studies conclude that there is no difference. Cigarette smoking is addictive, and some evidence suggests that women may have more difficulty quitting smoking than men.
Lung cancer in women versus lung cancer in men
Lung cancer in women is a biologically different disease than lung cancer in men.
Women may have genetic and biologic differences that affect the development of lung cancer, which include the following:
- Genes that cause women to be more vulnerable to the harmful effects of tobacco smoke
- Differences in how the chemicals in tobacco are metabolized (broken down) by the body
- Changes to genes that control cell growth, which may result in the development of cancer
- A decreased ability of the body to repair damaged DNA, as DNA damage can promote the development of cancer
- Hormones, such as estrogen, which could directly or indirectly affect cancer growth
Treatment and survival differences
Women with lung cancer live longer than men, again for reasons that are not yet understood. For example, the five-year relative survival rate (the percentage of people who survive at least five years after the cancer is detected) is higher in women: 16% compared with 12% in men. Women with early-stage lung cancer who have surgery to remove the tumor live longer than men, as do women who are treated for lung cancer that has spread outside the lung. A 2007 study found that older women with early-stage lung cancer live longer regardless of the type of treatment they received.
Other studies have found that some types of treatment work better in women with lung cancer. For example, cisplatin (Platinol)-based treatment seems to be more effective in women. Doctors have reported that women (along with never-smokers; patients with adenocarcinoma (cancer in lung cells that secrete substances); and those treated in Japan, China, and Korea) were most likely to benefit from a drug called gefitinib (Iressa). Gefitinib is available only to people who were already taking it, had taken it in the past and had a good effect, or as part of a clinical trial (research study involving people). Clinical trials are underway to study whether similar drugs, such as erlotinib (Tarceva), are also more effective in women never-smokers or former smokers.
On the horizon
Researchers are just beginning to understand how lung cancer is different in women, and how this difference affects lung cancer treatment and survival. Additional clinical trials are needed to learn more about preventing, diagnosing, and treating women with lung cancer.
More Information